Overview and Causes
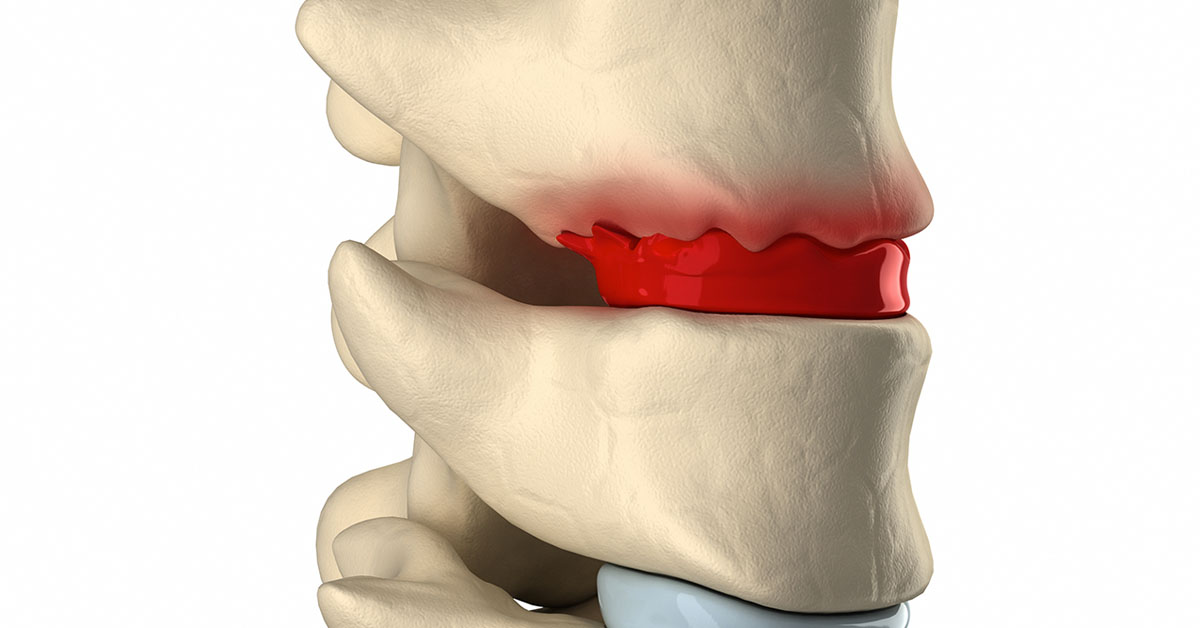
Degenerative Disc Disease (DDD) is the term used to describe the normal changes in the spinal discs as the body ages. Vertebrae, which make up the spine, are separated by the soft disks. These discs act as shock absorbers. This condition occurs when one of these disks weakens.
Despite the name, it is not actually a disease. But that does not mean the pain it causes is less real. It can be very painful and can affect quality of life to a great extent. Disc degeneration is a normal part of aging, but for some individuals, it can cause severe and chronic pain.
Following are some of the causes of degenerative disc disease:
The loss of fluid in the discs can be a cause. This makes the disk less flexible and reduces its ability to absorb shocks. This also reduces the distance between the vertebrae.
Annulus or capsule (the outer layer of disc) may be damaged or cracked. As a result the nucleus (jelly-like material inside the disc) may be forced to flow out of the cracks or tears. This may cause the disc to rupture, break into fragments or bulge.
A sudden injury to the disc can start disc degeneration
Smoking, heavy physical work and obesity can also cause degeneration.
Symptoms and Diagnosis
Symptoms of degenerative disc disease include:
Pain in lower back which radiates to hips
Pain in thighs or buttocks while walking
In some cases, irregular tingling or weakness through the knees
Pain in upper spine which may radiate to shoulders, arms and hands
This condition is diagnosed with a physical examination and a review of medical history. During physical examination, the surgeon looks for tenderness and changes related to nerves, for example changes in reflexes, numbness or tingling. Other conditions such as tumors, fractures and infections are also checked.
If symptoms of degenerative disc disease are suspected after initial examination, imaging tests may also be performed for diagnosis. These tests may include X-rays, MRIs or CT scans. Imaging tests are usually considered if the symptoms develop after injury or damage to nerves.
Treatment
Usually this condition can be successfully treated with non-surgical treatments. One or a combination of treatments like chiropractic manipulative therapy (CMT), physical therapy and anti-inflammatory medications can often provide relief.
Surgical treatment may be recommended if the non-surgical treatments fail to provide relief within two to three months. It may also be recommended if pain in legs or back restricts normal activity, if it is difficult to stand or walk, or if there is numbness or weakness in legs. Surgical treatment options include Anterior Cervical Discectomy with Fusion, Intervertebral Disc Annuloplasty, Intervertebral Disc Arthroplasty, etc.
Risks and Benefits
The draw back of non-surgical treatment is that it can be slow and take a long time to provide complete relief. The benefit is less disruption to the patient's routine life, as it does not require hospitalization or rehabilitation.
On the other hand, surgical treatments can be highly disruptive and they may require hospitalization and have activity restrictions for at least three to four weeks following surgery. Surgical treatment may be necessary if conservative treatments have not been successful or if the condition is too severe.